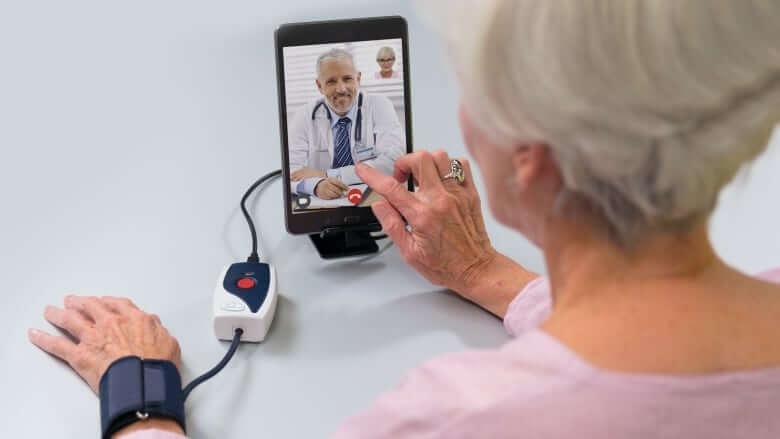
Post-surgery patients monitored virtually do better than those seeing doctors in person, study indicates
Patients who underwent non-elective surgery and used technology for remote monitoring had better outcomes a month after their release from hospital compared to people who were asked to go see their doctors for followup concerns, a new Canadian study has found.
Researchers from McMaster University in Hamilton followed 905 post-surgery patients from eight different hospitals in Ontario and Alberta for 30 days.
Of those, 451 were monitored remotely using a tablet computer provided to them to connect with a nurse daily for the first 15 days and then every other day for the remainder of the 30 days. Other items, like blood pressure cuffs and heart rate monitors, were connected to the tablet to measure blood pressure, heart rate, respiratory rate, oxygen saturation, temperature and body weight.
The other 454 were given the standard care — meaning they were told to see their doctor in a month or see their doctor if they had any problems.
The study monitored patients who were over age 40, with participants averaging age 63. It was completed during the early stages of the COVID-19 pandemic, between April and July 2020, and published in the British Medical Journal in September.
It found 30 per cent of people who were remotely monitored reported having medication errors, compared to six per cent of individuals who received traditional care.

“By using our intervention, we were able to correct those drug errors and have a dramatic impact,” said Dr. Philip J. Devereaux, one of the researchers, who is a cardiologist, clinical epidemiologist, and perioperative-care physician at Hamilton Health Sciences. He’s also the Salim Yusuf Chair in cardiology at McMaster University.
The study was funded through an innovation challenge application grant from pharmaceutical company Roche Canada as well as research grants from McMaster University, the Research Institute of St. Joseph’s Healthcare Hamilton, the Ottawa Hospital Academic Medical Association and the Queen’s University Department of Anaesthesiology and Department of Medicine Research, as well as in-kind support from the eight hospitals involved.
Cloud DX, a Kitchener-based tech company that created the software that monitored the patients, provided the tablets and data for the tablets used in the study at a discount and trained the medical professionals who took part.
Pain dealt with quickly
The study also found people who experienced pain had it addressed more quickly than the patients who received standard care.
Devereaux said many patients believe they have to live with pain, but the remote monitoring allowed nurses or doctors to advise patients on how to alleviate any discomfort they may be experiencing.
“We did it through a very simple intervention that is very low risk to patients, by increasing the use of acetaminophen, which is Tylenol. So we showed that there’s a safe way to dramatically decrease pain and moderate to severe pain is a very common and significant issue for patients after surgery,” Devereaux said.
Perhaps the best finding from the study, Devereaux said, was that for the hospitals that followed the protocols for when changes were noticed in patients — such as low or high blood pressure, or changes to heart rate or temperature — and escalated to a physician, “there was a very dramatic response in decreasing patients’ need to come back the emergency room or be readmitted to the hospital.”
This not only decreased costs to the hospital of patients coming back for emergency care, but also took stress off the health-care system while improving patient outcomes.
Ernst Seeger of Niagara Falls, Ont., was one of the patients who took part in the study after undergoing surgery for bladder cancer.
“Luckily for me, the good Lord blessed me,” Seeger said. “It was minuscule. It was very, very tiny. But [still] surgery.”
A nurse told him about the study and he opted to take part. Seeger said the remote monitoring helped him stay positive as he shared laughs with his doctors and nurses in regular check-ins.
“I felt like I was with family, you know, when I spoke to these people. And when I did have a little bit of a complication, I ended up getting an infection, which was very painful and wasn’t able to get in touch with the doctor.”
The pain was due to a urinary tract infection, but Seeger said it was dealt with quickly.
“The people from the medical centre turned around and got in touch with the pharmacist, and my prescription was waiting for me the very next morning,” he said.

“We enjoyed the moments that we had together, even though we didn’t know each other from a hole in the ground. They provided the service and they are providing a service that turns around, takes care of people when they’re ill,” he added.
“They have compassion and they care. All you have to do is pick that phone up and call.”
Kitchener-developed tech used
Cloud DX CEO Robert Kaul said they knew their technology worked and could be used in most off-the-shelf tablets, but they have struggled to get the medical community to give it a chance.

The researchers in this study “really laid out the map … laid the groundwork for the protocols that produce the best outcomes,” Kaul said.
“Change comes slowly to the health-care system. These studies are extremely important for the whole field because it gives us that base of knowledge and credibility to really have an impact over, you know, large populations. And of course, it takes lots of time, lots of effort, lots of energy to get this knowledge out to the world.”
Doctors want evidence tech helps patients
Devereaux said the pandemic shone a light on the need to ease pressure in the health-care system, and the study showed virtually monitoring a patient helped do that.
The need to help patients but also manage an influx of patients on a strained health-care system was echoed by Dr. Ann Collins, president of the Canadian Medical Association, earlier this year.
“Out of necessity, virtual care was adopted to preserve some form of access to care,” Collins said in a release in February. At the time, the CMA, the Royal College of Physicians and Surgeons of Canada, and the College of Family Physicians of Canada put forward 19 recommendations to accelerate the implementation of virtual care across the country. Those recommendations were not linked to the study published in the BMJ.
“Going forward, we need to make sure that virtual care is effectively integrated and delivered equitably. Our pivot to virtual care was swift and at times reliant on temporary measures that must now be made permanent and stable,” Collins said.
“Virtual care proved its value in the last year, so the opportunity is before us to make it an enduring facet of health care.”
Dr. Sonny Kohli, a critical-care physician at Oakville Trafalgar Memorial Hospital and co-founder of Cloud DX, said it can be difficult to encourage the health-care system to make changes. He found the results of the BMJ-published study “vindicating.”
“One of the challenges to disseminating technology like this is people want a ground truth evidence that there’s actually an impact on outcomes. And so [Devereaux’s] team has conducted the necessary clinical trials. It’s taken years to get here. But you know, necessity is the mother of invention,” Kohli said.
“[Devereaux] took an opportunity with the pandemic where his health-care system, Hamilton Health Sciences, was under a great strain and recognized as an opportunity here to see if this technology would have an impact on outcome.”

Kohli noted each hospital that took part in the study had a different approach to how it approved technology and changed the workflow. That means there’s no “blueprint” to make similar changes at every hospital.
“That’s another obstacle to the adoption of new systems for patient care,” he said, noting being part of the study is just another step in the process and now they need hospitals and health-care professionals to want to make changes.
“Once you overcome all that, I see a day where there’ll be many hospitals that are using this knowledge to better patient outcomes, but that there’s a lot of effort that still needs to take place for us to get there.”





Redes Sociais - Comentários